Transgender physiology refers to the physiological aspects of individuals who identify as transgender. Physiology encompasses the biological and physical characteristics of an individual, including their reproductive and sexual anatomy, hormone levels, and secondary sexual characteristics. Here are some key points regarding transgender physiology:
- Gender Identity: Gender identity is a deeply-held sense of being male, female, or something outside of the traditional binary gender categories. Transgender individuals have a gender identity that does not align with the sex they were assigned at birth.
- Assigned Sex at Birth: Assigned sex at birth is determined by physical characteristics such as external genitalia. Typically, individuals are assigned male or female based on this assessment, which may not align with their true gender identity.
- Hormones: Hormones play a significant role in transgender physiology. Many transgender individuals choose to undergo hormone therapy as part of their transition process. For male-to-female (MTF) individuals, hormone therapy often involves the use of estrogen and anti-androgens to develop feminine secondary sexual characteristics. Female-to-male (FTM) individuals may use testosterone to develop masculine secondary sexual characteristics.
- Secondary Sexual Characteristics: Secondary sexual characteristics are physical traits that differentiate between males and females but are not directly involved in reproduction. These include characteristics such as breast development, body fat distribution, facial hair growth, voice pitch, and muscle mass. Hormone therapy and other interventions can help transgender individuals develop secondary sexual characteristics that align with their gender identity.
- Reproductive Organs: Transgender individuals may or may not undergo surgeries to alter their reproductive organs to align with their gender identity. Female-to-male individuals may undergo procedures such as hysterectomy (removal of the uterus) and oophorectomy (removal of the ovaries), while male-to-female individuals may choose procedures such as orchiectomy (removal of the testes) and vaginoplasty (construction of a neovagina). These surgical interventions are personal choices and not all transgender individuals undergo them.
- Mental Health Considerations: Transgender individuals may face unique challenges related to their gender identity, including mental health concerns such as gender dysphoria. Gender dysphoria refers to distress or discomfort caused by the incongruence between an individual’s gender identity and assigned sex. Mental health support and access to transgender-affirming healthcare are crucial for transgender individuals’ overall well-being.
It’s important to remember that transgender physiology is diverse and varies among individuals. Not all transgender individuals will follow the same path or make the same choices regarding medical interventions or transition procedures. Each person’s journey is unique and should be respected. It is recommended to consult with qualified healthcare professionals who specialize in transgender healthcare for personalized guidance and support in understanding and addressing transgender physiology.
What are physiological changes in transgender?
Transgender individuals may undergo various physiological changes as part of their transition process. These changes can be influenced by hormone therapy, surgical interventions, and other gender-affirming treatments. It’s important to note that the specific physiological changes can vary between male-to-female (MTF) and female-to-male (FTM) individuals. Here are some common physiological changes associated with gender transition:
MTF (Male-to-Female) Transition:
- Hormonal Changes: MTF individuals undergoing hormone therapy typically take estrogen and anti-androgen medications. These hormones can lead to various changes, including:
- Breast development: Estrogen stimulates breast tissue growth, leading to the development of breasts.
- Softer skin: Estrogen can contribute to the softening of the skin texture.
- Decreased body hair growth: Anti-androgens help reduce body hair growth, making it less dense and coarse.
- Redistribution of body fat: Fat tends to redistribute to the hips, thighs, and buttocks, resulting in a more feminine body shape.
- Reduced muscle mass: Testosterone levels decrease, leading to a decrease in muscle mass and strength.
- Emotional and Mental Well-being: Many MTF individuals report improvements in emotional well-being and a reduction in gender dysphoria as they align their external appearance with their gender identity.
FTM (Female-to-Male) Transition:
- Hormonal Changes: FTM individuals undergoing hormone therapy typically take testosterone. Some physiological changes associated with testosterone therapy include:
- Facial hair growth: Testosterone can stimulate the growth of facial hair, including beard and mustache.
- Deepened voice: Testosterone causes the vocal cords to thicken, resulting in a deepening of the voice.
- Increased muscle mass: Testosterone promotes the development of lean muscle mass and increased strength.
- Body hair growth: Hair growth on the chest, arms, legs, and other areas can become more pronounced.
- Fat redistribution: Fat distribution tends to shift towards a more masculine pattern, with less fat accumulating in the hips and thighs.
- Top Surgery: FTM individuals may choose to undergo “top surgery” to remove breast tissue and create a more masculine chest appearance. This procedure is often done through mastectomy or chest reconstruction.
- Emotional and Mental Well-being: Similar to MTF individuals, FTM individuals often experience improved emotional well-being and a reduction in gender dysphoria as they align their physical appearance with their gender identity.
It’s important to remember that the physiological changes mentioned above are general observations, and the specific effects can vary from person to person. Additionally, not all transgender individuals pursue medical interventions or undergo the same procedures. The decision to undergo hormone therapy, surgery, or other treatments is personal and should be made in consultation with qualified healthcare professionals who specialize in transgender healthcare.
Which hormone is present in transgender?
The choice to use hormone therapy in transgender individuals depends on their desired gender identity and the direction of their transition. Hormone therapy involves the use of hormones to promote physical changes that align with an individual’s gender identity. Here are the commonly used hormones in transgender hormone therapy:
- Estrogen: Estrogen is the primary hormone used in feminizing hormone therapy for transgender women (male-to-female individuals). It is typically administered in the form of estradiol. Estrogen helps promote the development of feminine secondary sexual characteristics such as breast growth, softer skin, decreased body hair growth, and fat redistribution.
- Anti-Androgens: Anti-androgens are often used in conjunction with estrogen in feminizing hormone therapy. They work by blocking or reducing the effects of testosterone. Commonly used anti-androgens include spironolactone, cyproterone acetate, and bicalutamide. By suppressing testosterone levels, anti-androgens help inhibit masculine features like body hair growth and muscle mass development.
- Testosterone: Testosterone is the primary hormone used in masculinizing hormone therapy for transgender men (female-to-male individuals). It is usually administered as injectable testosterone or in other forms such as gels or patches. Testosterone promotes the development of masculine secondary sexual characteristics, including facial and body hair growth, voice deepening, increased muscle mass and strength, and fat redistribution.
It’s important to note that hormone therapy is typically initiated under the supervision of qualified healthcare professionals, such as endocrinologists or specialized transgender healthcare providers. The specific regimen, dosage, and monitoring can vary based on individual factors such as age, overall health, and medical history. Hormone therapy should be carefully managed and regularly monitored to ensure the safety and effectiveness of the treatment.
What are the biological causes of transgenderism?
The exact biological causes of transgenderism, also known as gender dysphoria or gender incongruence, are not fully understood. Current research suggests that a combination of genetic, hormonal, and neurological factors may contribute to the development of gender identity that differs from the sex assigned at birth. However, it’s important to note that the understanding of transgenderism is still evolving, and more research is needed to fully elucidate its biological underpinnings. Here are some factors that have been studied and proposed as potential contributors:
- Genetic Factors: Studies have indicated that there may be a genetic component to transgender identity. Some research suggests that certain genes or variations in gene expression patterns could influence an individual’s gender identity development. However, the specific genes involved and their mechanisms of action are not yet fully understood.
- Hormonal Influences: Hormonal factors during prenatal development have been hypothesized to play a role in shaping gender identity. The timing and levels of sex hormones, such as testosterone and estrogen, during critical periods of fetal brain development, may contribute to the differentiation of gender identity. Variations in hormone exposure or response could potentially influence the development of transgender identities.
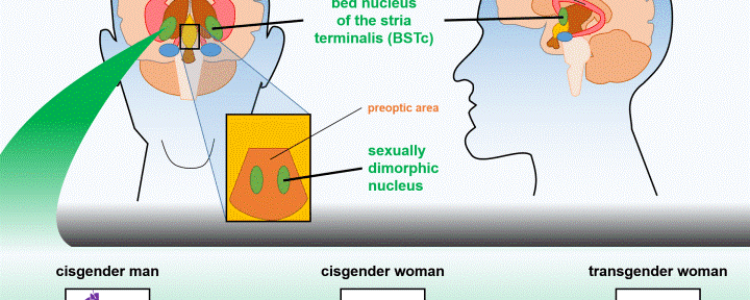
- Brain Structure and Function: Studies using neuroimaging techniques have shown differences in brain structure and functional connectivity between cisgender individuals (those whose gender identity aligns with their assigned sex at birth) and transgender individuals. These differences, particularly in regions associated with gender identity and body perception, suggest that neurobiological factors may be involved in transgender identity development.
It’s important to emphasize that transgenderism is not a result of personal choice or external influences. Rather, it is understood as a deeply-held sense of gender identity that may differ from societal expectations or assigned sex at birth. While biological factors may contribute to gender identity development, they interact with a complex interplay of psychological, social, and environmental factors.
It’s also crucial to note that being transgender is not considered a disorder or pathology. It is recognized as a valid variation of human diversity, and the focus of medical and psychological care is on providing support, affirmation, and access to appropriate healthcare for transgender individuals. Understanding the biological underpinnings of transgenderism can contribute to the development of more informed and inclusive approaches to transgender healthcare.
What is the physical anatomy of transgender?
The physical anatomy of transgender individuals can vary depending on their gender identity, the stage of their transition, and any medical interventions they may have undergone. It’s important to recognize that transgender people have diverse experiences, and not all transgender individuals pursue or undergo medical interventions or surgeries. Here is a general overview of the physical anatomy for transgender individuals in relation to their gender identity:
- Male-to-Female (MTF) Transgender Individuals:
- Assigned Sex at Birth: MTF individuals are assigned male at birth based on their external genitalia.
- Primary Sexual Characteristics: MTF individuals have male reproductive organs, including a penis and testes. However, some individuals may undergo genital reconstruction surgery, known as vaginoplasty, to create a neovagina.
- Secondary Sexual Characteristics: Prior to hormone therapy, MTF individuals typically develop masculine secondary sexual characteristics such as facial and body hair, a deeper voice, and a more masculine body shape. Hormone therapy, including estrogen and anti-androgens, can help develop feminine secondary sexual characteristics such as breast growth, softer skin, and fat redistribution.
- Female-to-Male (FTM) Transgender Individuals:
- Assigned Sex at Birth: FTM individuals are assigned female at birth based on their external genitalia.
- Primary Sexual Characteristics: FTM individuals have female reproductive organs, including ovaries, a uterus, and a vagina. Some individuals may undergo procedures such as hysterectomy (removal of the uterus) and oophorectomy (removal of the ovaries) as part of their transition.
- Secondary Sexual Characteristics: FTM individuals typically develop feminine secondary sexual characteristics during puberty, including breast development and wider hips. Hormone therapy with testosterone can induce the development of masculine secondary sexual characteristics such as facial and body hair growth, voice deepening, increased muscle mass, and fat redistribution.
It’s important to note that not all transgender individuals pursue medical interventions or surgeries to modify their physical anatomy. Each person’s transition journey is unique and personal decisions regarding medical interventions are made based on individual needs, desires, and access to healthcare.
It’s also essential to approach discussions about transgender anatomy with sensitivity and respect. It’s recommended to use appropriate language and to respect individuals’ privacy and autonomy regarding their bodies and personal experiences.
The physiology of transgender people can vary depending on the individual’s gender identity, the type of gender-affirming care they receive, and their overall health. However, there are some general physiological differences between transgender people and cisgender people (people whose gender identity matches their sex assigned at birth).
For example, transgender women who take estrogen may experience changes in their body fat distribution, breast development, and skin texture. Transgender men who take testosterone may experience changes in their body hair growth, muscle mass, and voice pitch. These changes are due to the effects of hormones on the body.
Transgender people who have undergone gender-affirming surgery may also experience physiological changes. For example, transgender women who have undergone top surgery (breast removal) may experience changes in their breathing and range of motion. Transgender men who have undergone bottom surgery (genital reconstruction) may experience changes in their sexual function.
It is important to note that not all transgender people choose to undergo gender-affirming care. Some transgender people may only experience social transition, which involves changing their name, pronouns, and clothing to match their gender identity. Others may choose to undergo hormone therapy or surgery, or a combination of both.
The physiological changes that transgender people experience can vary depending on the individual. However, these changes can be an important part of the gender-affirming process for many transgender people.
Here are some additional resources that you may find helpful:
- The Trevor Project: https://www.thetrevorproject.org/: A national organization that provides crisis intervention and suicide prevention services to LGBTQ youth
- GLAAD: https://www.glaad.org/: An organization that works to promote acceptance of LGBTQ people
- Human Rights Campaign: https://www.hrc.org/: An organization that works to achieve equality for LGBTQ people in all areas of life